2025 NIKTT Gathering

To get the most out of this report, please use the navigation bar at the top of the page to scroll through different sections.
Aboriginal and Torres Strait Islander people should be aware that this report contains images of people who have passed away.
Photography featured in this report is credited to Colleen Raven Strangways, Nharla Media


Acknowledging Country.
The National Indigenous Kidney Transplantation Taskforce acknowledges the Country, Custodians, and Community of the lands, seas, and skies upon which we live, work, travel, and gather.
The 2025 NIKTT Gathering was held on the traditional Country of the Kaurna people of the Adelaide Plains.
We acknowledge and thank the Custodians who welcomed us to Country, and acknowledge our privilege in being able to share and learn on Kaurna Yarta.
Sovereignty was never ceded.
This always was, and always will be, Aboriginal land.
Background.

Aboriginal and Torres Strait Islander people experience end-stage kidney disease at much higher rates than non-Indigenous people, yet are far less likely to be waitlisted for a transplant and therefore less likely to receive one.
In 2018, the Transplantation Society of Australia and New Zealand (TSANZ) released a report containing 35 recommendations to improve access to kidney transplantation for Aboriginal and Torres Strait Islander people.
Many of these recommendations were directed at Commonwealth, State, and Territory governments, while others needed leadership from a national body.
At the top of the list of TSANZ recommendations was a call for the Commonwealth Government to establish the National Indigenous Kidney Transplantation Taskforce.
A conference was held in Alice Springs in 2019, the National Indigenous Dialysis and Transplantation Conference, as the first national meeting of this NIKTT group.
It was led by Co-Chairs of the Taskforce, Professor Jaquelyne Hughes and Professor Stephen McDonald AM.
The NIKTT was comprised of 35 members, with a range of First Nations people and non-Indigenous allies, and patients, clinicians, and organisational stakeholders.
The NIKTT was tasked with looking at three of the TSANZ recommendations:
- Enhance data collection around waitlisting
- Investigate cultural bias in kidney care settings
- Pilot models of care that could improve access to the waitlist
After three years of work, the NIKTT's first round of funding and activities came to an end. The Taskforce had successfully established Indigenous Reference Groups at transplant units; it had piloted eight different projects across Australia; it had commissioned a report on cultural bias in kidney care; and it had expanded data collection at renal units to understand why people weren't being waitlisted.
To share this work, the NIKTT held the first NIKTT Transplantation Equity Gathering in December 2022. The Gathering's aim was to bring together the people on the Taskforce alongside patients and Community members who had been involved in NIKTT activities.
The 2022 Gathering showcased what had been achieved across the three recommendations, highlighting the models of care that worked and encouraging conversations about what else needed to be done.
A key outcome of the Gathering was the collective writing and endorsement of a Position Statement on transplantation equity.
This statement called for the continuation of the NIKTT and the continuation of the momentum built by all those involved in NIKTT work.
This Position Statement, as well as the overall recommendations from the Taskforce, were presented to federal ministers in early 2023.
As a direct result of this advocacy and sharing of knowledge gained, the Commonwealth Government provided bridging funding for the NIKTT Secretariat to continue work for one year (2024).
This funding aimed to progress improvements in access to kidney transplantation for Aboriginal and Torres Strait Islander peoples through:
- Supporting the continued development of Indigenous Reference Groups at transplant units;
- Developing a national data dashboard to track equity;
- Developing a proposed national body to lead equity work; and
- Convening a second national Gathering.
The 2025 Gathering was therefore a key activity and outcome of continued NIKTT work. It aimed to bring together once again the people involved in the Taskforce alongside the patients and family the work seeks to support.
The Gathering set out to celebrate the dedication and efforts underway across the country to advance transplantation equity for Aboriginal and Torres Strait Islander people, while keeping conversations centred on what our communities believe must happen next to drive meaningful change.
This report highlights the stories shared at the Gathering as well as the Priorities and Actions noted throughout the three days. To read the full report, with detailed information on each presentation given, please download the PDF below.
Designing the Gathering

The Gathering was designed to be culturally safe, inclusive, and actively engaging.
We took an intentional approach to participation, beginning with an invitation list that prioritised geographic diversity, a range of perspectives and experiences, and the inclusion of new voices who had not attended the 2022 Gathering.
For patients and their carers, the NIKTT covered all travel, accommodation, and meal costs to ensure they could attend the Gathering without financial burden.
For NIKTT stakeholders and other professionals working in transplantation and renal care, we asked attendees to complete a short Expression of Interest form. As we explicitly designed the 2025 Gathering to be a space dedicated to championing Aboriginal and Torres Strait Islander leadership, knowledge, and self-determination, the EOI process aimed to uphold the integrity of this Blak-led space by encouraging potential attendees to reflect on their engagement prior to registration. We asked people to complete four short questions to demonstrate their commitment to engaging respectfully, contributing meaningfully, and participating as active learners.
All potential attendees were asked to review and commit to the event’s guiding principles before confirming their desire to attend. This was a deliberate step to ensure the Gathering brought together people who were willing to engage fully and contribute to collective action.
Everyone was asked to come with an open mind, to listen deeply, and to speak plainly. Practical guidelines – such as one speaker at a time, no blame or shame, and leaving ego at the door – sought to create a respectful space. While it was acknowledged that many might find it important to discuss challenges, we emphasised that the focus remained on finding shared, actionable solutions.
Cultural safety was a non-negotiable. Participants were expected to be mindful of language, respectful of difference, and responsive to the diverse ways of knowing, being, and doing represented in the room.


The following sections provide an overview of the program across the Gathering’s three days.
We then summarise the key priorities and calls to action that emerged throughout the event.
To jump to a different section or return to one, use the navigation bar at the top of your screen.
To read a detailed account of each presentation and discussion, please visit www.niktt.com.au/gathering2025
Day One: Gather
Aim: To create a dedicated space for Aboriginal and Torres Strait Islander patients, carers, families, health workforce, and leaders to share experiences, celebrate successes, and identify challenges and opportunities in kidney transplantation equity

In response to strong demand at the 2022 Gathering for more patient and provider stories, the 2025 Gathering was held over three days, from 18–20 February.
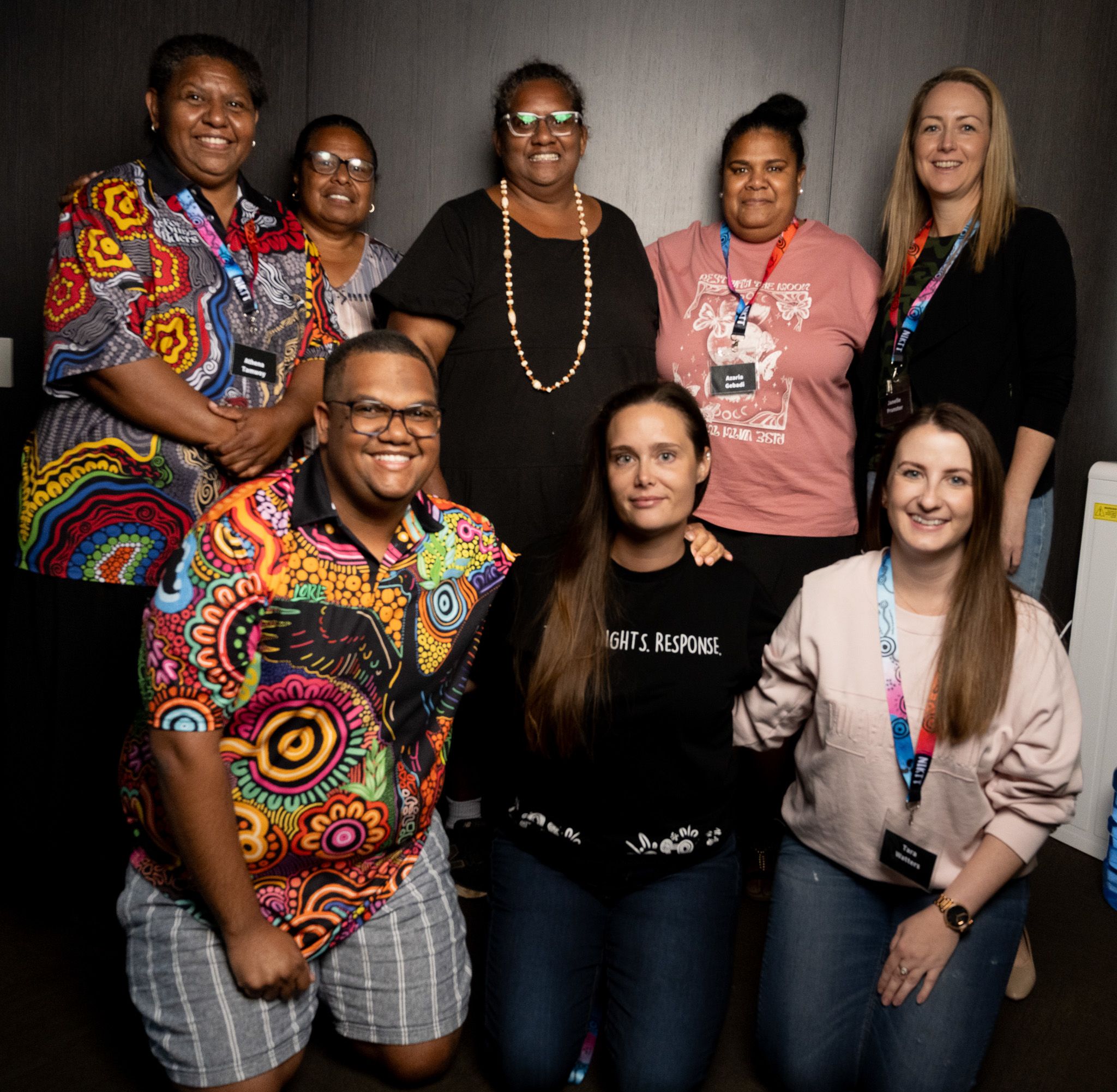
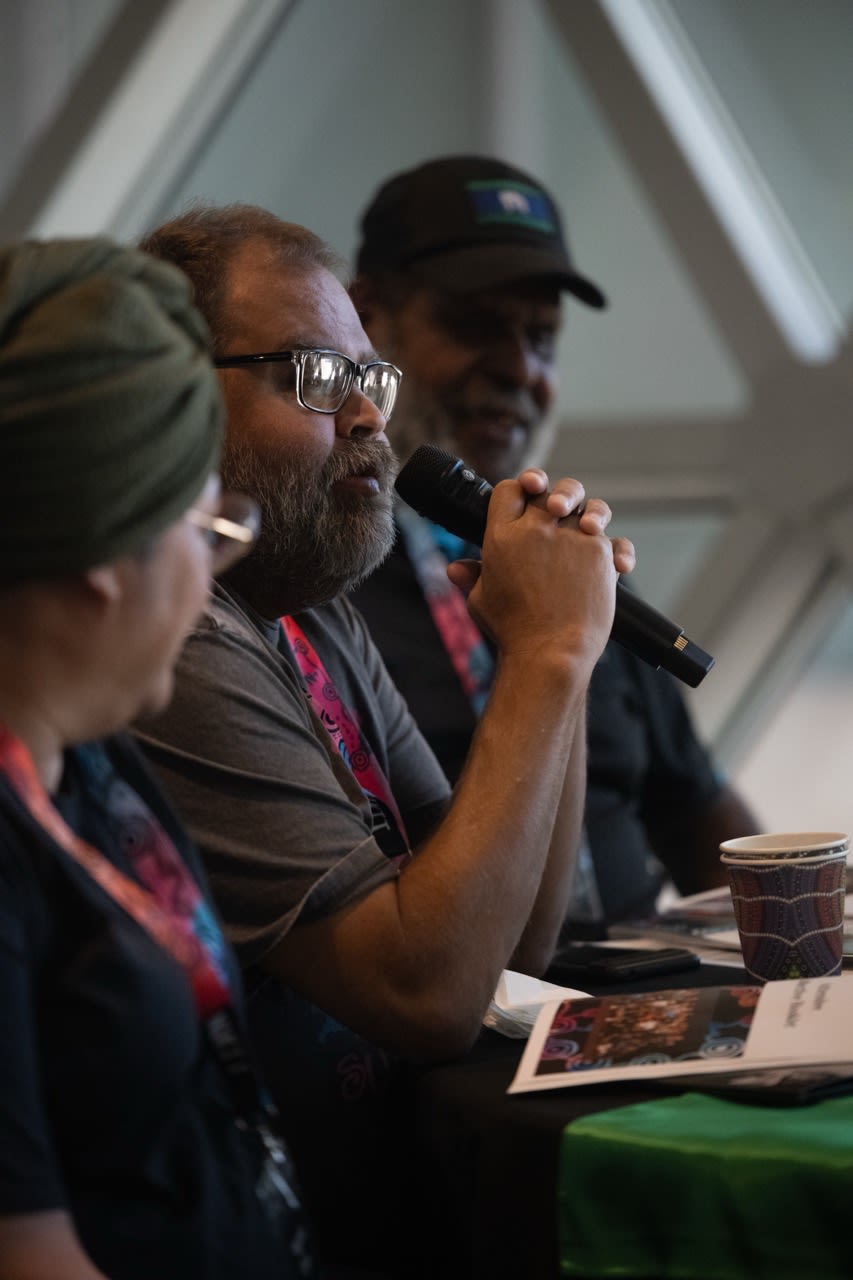
The first day of the Gathering was a dedicated Blak space. It provided a closed space for Mob to connect, share experiences, and begin shaping priorities for the future.
The day opened with a Welcome to Country by Ashum Owen, a Kaurna, Ngarrindjeri, and Narungga woman and leader of Ngangki Warra — a female-led cultural group that amplifies women’s voices through culture, dance, and language.
The Welcome was followed by an introduction to the purpose of the Gathering and a round of introductions among attendees. The morning and early afternoon centred on shared storytelling, with participants invited to reflect on their own journeys, sharing perspectives on what does, and does not, work for people in their regions for kidney transplant care.
In the afternoon, discussions continued with a session introducing the ANZDATA Aboriginal and Torres Strait Islander Health Working Group, and the final session brought together themes from across the day, with each region nominating a Kidney Champion to speak on their behalf in the cross-sector sessions planned for Day Two.
Because all sessions on Day One were Mob-only, with the space intentionally held for open, grounded discussion among Community, no recordings were made from this day and quotes, themes, or key discussion points were not collated.
While the content of Day 1 wasn’t recorded, the photos below offer a glimpse into the space and moments shared.
Scroll to the left and right to see more.
Day Two: Reflect
Aim: To bring the kidney community together from all jurisdictions to share knowledge, highlight achievements, and discuss practical strategies to improve access to transplantation and kidney care

Day Two began with a heartfelt and powerful Welcome to Kaurna Yarta by Jakirah Telfer, who comes from the dry forest clan, Mullawirra Meyunna, of the Kaurna people of the Adelaide plains region. Speaking first in language, Jakirah acknowledged the ancient spirits that remain present on Kaurna land and the living culture that continues to breathe through the people today. She welcomed delegates to Tarntanyangga, the dreaming place of the red kangaroo.
“This is my country and this country is my bloodline. The songs of the land echo on the waters of my coast and carry on the winds the voices of the old people. What I just said in language is acknowledging the ancient that still lays sleeping here, but also the culture that still lives and breathes through us.”
Jakirah Telfer
Introduction to NIKTT: Where Have We Come From, Where Are We Going?
Professors Stephen McDonald and Jaquelyne Hughes opened the core sessions of Day 2 by providing a foundational overview of the NIKTT, tracing its evolution, outlining its core activities, and highlighting its ongoing role in advocating for systems change.
They emphasised that Australia’s kidney care system already possesses the clinical tools and infrastructure needed to support people with kidney failure through to transplantation.
They highlighted that the challenges we see in transplantation access lie not in medical capability, but in ensuring equitable access to systems.
As Professor McDonald explained, NIKTT was established not just to describe these inequities but to actively demonstrate how to overcome them. Through pilot projects, enhanced data collection, and Indigenous-led governance, NIKTT provided both proof-of-concept and pathways forward:
“One of the key things that NIKTT was set up to do was to start a process of fixing it — of showing how to fix it, and what the fixes looked like.” - Professor McDonald
The results of NIKTT work were published as a special supplement in the Medical Journal of Australia in October 2023.
NIKTT and other key stakeholders were invited throughout 2023 and 2024 to meet with the Federal Department of Health to provide insight into the National Strategy for Organ Donation, Retrieval, and Transplantation.
Professors Hughes and McDonald noted that while the government’s National Strategy acknowledges the importance of equity and prioritising access to transplantation, it currently lacks an implementation plan.
They concluded by highlighting the opportunity — and responsibility — for the Gathering participants to collectively shape what happens next.
"There is a clear national strategy, and in that, the Federal Government has said that Priority Area number two is actually fixing this problem [of inequitable access to transplantation for Aboriginal and Torres Strait Islander people].
"It is not priority 23, it is right up there at the top... [However,] there is no implementation plan for this document.
“[But] that’s the opportunity. The document says “we're not sure what to do. The work of the NIKTT will inform implementation.”
"What that means is the power is in [this] room. People in Canberra know they need to do something. They don't quite know what and how to do it. And that's called an opportunity.” - Professor McDonald
Sharing Stories: South Australia
Central and Northern Adelaide Renal Transplant Services (CNARTS)
Presenters: Kelli Karrikarringka Owen, Kate Tyrell, Sam Bateman, Richard Goldsmith, Arna Westhead, Donna Vigor
The CNARTS team presented their approach to embedding cultural leadership and Aboriginal governance in kidney care. Led by Aboriginal and non-Aboriginal staff working together, the team described their model at the Royal Adelaide Hospital (RAH), which combines clinical expertise, cultural authority, and place-based learning. The work is guided by the Indigenous Reference Group Purdita Purruna Wangkanthi (“Talking Kidney Health”), formed with NIKTT support and now funded directly by the hospital. The IRG identified eight priority areas for improving cultural safety; the team has begun actioning the first three, including a culturally safe model of care, ongoing engagement with Kaurna Elders, and the introduction of traditional healing practices such as organ cleansing ceremonies.
A key aspect of the model is the formal integration of cultural leadership into the clinical system. Kelli Karrikarringka Owen, a transplant recipient and Aboriginal leader, holds a designated cultural advisory role within the unit. Alongside her, a multidisciplinary “Kidney Dream Team” supports co-design and long-term change. The service has grown its Aboriginal workforce from one to six staff, introducing new roles such as a Patient Navigator Coordinator, an Aboriginal Health Practitioner, and COMPASS Patient Navigators with lived experience. These roles aim to provide responsive, community-informed support throughout the kidney care journey.
To build broader cultural safety, the team developed “Walking in Two Worlds,” a training course for hospital staff that focuses on place-based learning and challenges default assumptions about Aboriginal patient experiences. The course uses Kaurna Yarta to explore how health, culture, and Country intersect, and encourages staff to identify and address systemic barriers to care. While not intended for direct replication, the team encouraged other hospitals to develop their own culturally relevant programs in partnership with local Elders and Communities.
The presentation also identified future priorities, including succession planning for team roles, expanding workforce pathways, developing educational materials in Language, and progressing the remaining IRG priorities.
Sharing Stories: Western Australia
Kimberley Renal Services (KRS)
Presenters: Emma Griffiths and Nick Corsair
KRS, a community-controlled service based in Broome, shared their work in increasing transplant suitability assessments and embedding these into local models of care. They presented a continuous quality improvement initiative designed to ensure all dialysis patients received systematic transplant suitability assessments. The team developed a tool that enabled local GPs and staff to classify patients as ready, delayed, or currently unsuitable for transplant, with regular review by visiting nephrologists.
Of 66 patients assessed, the majority were found to have no permanent contraindications. Many had temporary barriers such as smoking or weight that could be addressed with support. Within 12 months, eight patients were added to the transplant waitlist.
The team also conducted interviews with patients and staff, identifying key themes:
1. People wanted more information
Participants wanted to know more about the transplant process. They wanted more time with the transplant coordinator and then more follow up from the transplant team. They wanted lists of what needed to be done and where to get support,
2. People felt they were always waiting or forgotten
Some patients felt like they were waiting a while to hear back or proceed to do further testing. While some patient progressed others did not and left patients with a feeling or either being left out or having no idea of what was happening.
3. People knowing what, but not how, to make changes
A large challenge for those aware of what was stopping them getting on the waitlist, like weight loss and giving up smoking, weren’t sure where to get support. More promotion and education on making change were identified as helpful.
KRS highlighted ongoing work to embed transplant processes into routine care, including hiring more staff, developing peer education models, and integrating transplant assessments into their electronic medical record. They noted the value of transplant recipients accompanying outreach trips, and flagged future priorities including post-transplant care models and capacity-building in local health services.
Sharing Stories: Northern Territory
Alice Springs Renal Unit
Presenter: Kerry Dole
Kerry Dole, Renal Transplant Coordinator, presented on the development of the THRIVE model in Alice Springs — a patient-centred approach to dialysis with the ultimate goal of increasing transplant access for First Nations patients in Central Australia. THRIVE reframes dialysis as a space for growth, learning, and empowerment, rather than passive treatment. It is grounded in a strengths-based framework and co-designed with patients and clinicians.
The THRIVE model includes:
Training: Skills-building around kidney health and self-management
Honouring: Valuing patients’ strengths and experiences in shaping their care
Resourcing: Supporting patients to become advocates and educators
Inviting independence: Encouraging participation in self-care and decision-making
Vehicle to transplantation: Supporting transplant readiness and follow-up
Empowerment: Enabling patients to lead their care and influence others
The model is currently being piloted with a small group of self-nominated patients, with long-term plans for expansion. To make this model sustainable, Ms Dole identified the need for:
- Ongoing nephrologist time dedicated to the project,
- Partnerships with Aboriginal Community Controlled Health Organisations (e.g., Congress, Purple House),
- Aboriginal Health Practitioner and Patient Navigator roles embedded within government services, and
- Research partnerships to support evaluation and scale-up.
Ms Dole also shared findings from a retrospective transplant outcomes study in Central Australia, led by Dr Sajan Thomas, which showed improvements in Aboriginal and Torres Strait Islander patient and graft survival post-2015, particularly in the first five years after transplant.
Sharing Stories: Queensland
North Queensland Kidney Transplant Service (NQKTS)
Presenter: Michelle Harfield
Dr Michelle Harfield introduced the establishment of Queensland’s second kidney transplant service, based at Townsville University Hospital, due to begin performing transplants in 2025. Designed to serve North and Far North Queensland, the service is being built from the ground up with cultural safety, regional equity, and sustainability at its core. Dr Harfield described the deliberate effort to embed values of equity and cultural respect across governance, care delivery, staffing, and evaluation — guided by recommendations from NIKTT’s performance and cultural bias reports.
The model includes:
- Recurrent funding for an Indigenous Reference Group co-designed with community members and chaired by Indigenous health leaders, recognised as subject matter experts,
- Dedicated Aboriginal and Torres Strait Islander health workforce embedded within the transplant service (not seconded to other areas), to establish a strong, regionally-based transplant capability,
- Cultural information tools used at referral to capture individual needs related to housing, health literacy, spirituality, and support systems,
- Outreach clinics and a proposed one-stop “investigation day” model to reduce patient travel burden, and
- Evaluation structures, including key performance indicators related to patient displacement from Country, completion of cultural tools, and feedback from patients, workforce, and Community.
Dr Harfield noted that strong political momentum in Queensland enabled the successful case for recurrent funding, and stressed that future sustainability depends on embedding values into structure and policy. She closed by acknowledging the importance of building upon existing work from the Princess Alexandra Hospital and NIKTT’s outreach clinics, with the goal of creating a transplant service that reflects what patients say they want.
Sharing Stories: National
Better Renal Services
Presenter: Melanie Beacroft and Jason Agostino
Melanie Beacroft and Dr Jason Agostino presented on the Better Renal Services initiative — a national effort to improve dialysis access for Aboriginal and Torres Strait Islander people in remote and very remote areas. The program, funded by the Australian Government, is guided by the National Agreement on Closing the Gap and aims to deliver culturally responsive, community-led care.
Key features of the initiative:
- $73.2 million was committed to build 30 four-chair dialysis units with workforce accommodation as needed, based on local need and community readiness,
- A Steering Committee, co-chaired by Ms Beacroft and Dr Agostino, includes representatives from Aboriginal and Torres Strait Islander organisations, kidney experts, and governments to guide site selection and planning, and
- To date, nine units have been funded, including completed infrastructure in Coober Pedy and a developing project on Badu Island.
Dr Agostino emphasised that infrastructure alone is insufficient:
“It’s one thing to build a couple of buildings, it’s another thing to have the appropriate staff there and to fund it appropriately so that it’s sustainable.”
He called out the unsustainable reliance on charity and short-term funding, stressing the need to embed local Aboriginal and Torres Strait Islander health workforces into these services for long-term success.
Dr Agostino also described NACCHO’s work to develop a national strategy addressing the “triple threat” of kidney disease, diabetes, and cardiovascular disease. This strategy will:
- Be informed by consultations with 146 Aboriginal Community Controlled Health Organisations (ACCHOs),
- Span the full continuum of care from prevention to palliative care, and
- Include targeted health workforce upskilling, including kidney care modules developed with Aboriginal training organisations and the Kimberley renal team.
A related workforce initiative is the Aboriginal and Torres Strait Islander Health Traineeships program, which has seen nearly 400 enrolments to date, offering a platform for future specialisation in areas like kidney care.






Day Three: Act
Aim: To review identified gaps and opportunities, and reach a consensus on priorities for advancing kidney transplantation equity

The final day of the Gathering brought together the full group of participants to focus on priority-setting, system change, and future directions.
The day began with a powerful and unexpected performance: a live enactment of a transplant phone call by Richard Jenkins, a transplant recipient from Western Australia, and Dr Andrew Mallet, a nephrologist from Queensland.
Framed by Professor Hughes as a way to centre lived experience and “invite people into the space,” the performance illustrated the emotional weight and significance of receiving a transplant offer.
View an animation of the call, with the audio taken directly from the Gathering performance:
Session 1: TSANZ Revised Allocation Algorithm: Kidney Only Allocation Algorithm
Presenter: Kate Wyburn
Dr Kate Wyburn, clinical transplant nephrologist and president of the Transplantation Society of Australia and New Zealand (TSANZ), presented an overview of the revised Kidney Only Allocation Algorithm (KOALA). She opened by acknowledging the significance of the role-played transplant phone call in grounding technical information in real patient experiences.
Kate explained that the kidney allocation system is a computer-based algorithm that determines which patient on the waitlist will receive an available donor kidney. While the previous system was applied equally, it produced unintended inequities. The revised algorithm aims to improve fairness, transparency, and clinical outcomes through six core changes:
- Better support for sensitised patients – Uses a graded scale to ensure those with high antibody levels (due to previous transplants, transfusions, or pregnancy) are not disadvantaged
- Improved prognosis matching – Seeks to match donor kidneys to recipients based on predicted longevity, maximising overall life years gained
- Support for younger patients – Prioritises children and young adults through extended paediatric priority and better HLA matching to reduce long-term sensitisation
- Adjustment for matchability by ethnicity – Considers the difficulty of finding matches for patients with rarer immune profiles, rather than relying on fixed six-antigen matches
- Retention of time-based equity – Time on the waitlist remains a central factor once clinical factors are addressed
- Shift from tiered to continuous scoring – Replaces rigid thresholds (e.g., PRA >95%) with a continuous score, allowing for more tailored and equitable decision-making.
Kate highlighted that allocation is only one part of the transplant journey, and that getting onto the waitlist remains the greatest barrier. She emphasised the importance of early education, staying well, and ensuring patients understand what to expect — including the possibility of travel for a transplant that may not go ahead.
Session 2: National Transplant Strategy
Presenter: Rushika Wirasinha
Rushika Wirasinha, Director of the Organ and Tissue Policy and Programs Team at the Australian Government Department of Health and Aged Care, presented an overview of the National Strategy for Organ Donation, Retrieval and Transplantation, released in November 2024. She opened by sharing her personal journey from Sri Lanka to Canberra, and her path from medical research into health policy, framing her work as a way of translating practical ideas into systemic change.
The strategy was endorsed by all state, territory, and federal health ministers and sets out four national priorities and ten goals aimed at improving the organ donation and transplantation system. While the strategy does not include dedicated funding at this stage, its multi-jurisdictional endorsement provides a mandate for coordinated implementation and future investment.
Ms Wirasinha focused particularly on Priority 2, which seeks to improve equitable access to transplantation for Aboriginal and Torres Strait Islander peoples and people in regional and remote areas. She acknowledged the NIKTT’s leadership in shaping this priority and stated that her team has worked closely with the Taskforce to develop an initial proposal to support its implementation — one that will continue to be refined in response to Gathering outcomes and broader consultation. She also referenced Priority 1 (system coordination and living donation) as relevant, while reaffirming that Priority 2 remains the primary avenue for embedding equity and Aboriginal and Torres Strait Islander governance.
Looking ahead, the Joint Organ and Tissue Steering Committee (JOTSC) will be responsible for developing an implementation plan for the National Strategy. This plan will outline a mix of immediate and longer-term actions, some dependent on future budget decisions. Ms Wirasinha acknowledged that while there are constraints ahead of the next federal election, (held in May 2025) there are still opportunities to build momentum and prepare funding proposals for upcoming budget cycles.
Following the presentation, Kelli Owen raised concerns about the lack of immediate funding and the absence of a clear implementation pathway:
“Our people are still dying on these machines. Our people are very sick and we are pushing through as hard as we can – and we hear that you are hearing us, but what do we now need to do if there is no way forward and no resourcing and no implementation plan?”
Ms Wirasinha acknowledged the frustration, reiterating that funding decisions are made by government and that this year presents an opportunity to build awareness and momentum toward future implementation. She encouraged participants to continue raising the profile of this work in their communities and through conversations with local representatives.
Following the opening sessions, Day 3 continued with interactive workshops on priority setting and confirming the Position Statement.
Read on to find out the outcomes from the 2025 Gathering.



Priorities
The following priorities were collated from feedback across all three days of the Gathering

Attendee Priorities, Grouped by Theme
Aboriginal and Torres Strait Islander workforce and leadership
Participants repeatedly emphasised the need to grow and support an Aboriginal and Torres Strait Islander workforce across clinical, community, and peer roles. This included calls for peer navigators, rural workforce development, and more Indigenous leadership in decision-making and governance structures. Indigenous Reference Groups were also seen as vital, with requests for consistent national coordination and long-term investment.
Cultural safety and better communication
A central concern was the lack of cultural safety within the health system. Participants called for place-based cultural safety training, better understanding of cultural practices and protocols, and tools like the Clinical Yarning Model to be embedded in practice. Many shared personal experiences of disrespectful language and communication, with strong calls for systemic accountability. The need for health services to understand and speak respectfully to Aboriginal and Torres Strait Islander people was a recurring theme.
Education and resources
There was widespread support for culturally appropriate education resources that explain the transplant journey and broader kidney care pathway in clear, accessible formats. Resources should be in-language, visual, and suitable for all ages. A centralised national hub was proposed to ensure access to up-to-date, reliable information for patients, carers, and clinicians.
Access to care
Participants spoke of the difficulties accessing early transplant workup, dental care, and specialist appointments. They proposed expanded mobile dialysis access (e.g. trucks), more dialysis chairs in community, and increased outreach models for transplant assessment.
Psychosocial, carer, and family support
Caring for the carer was raised by many participants. Attendees stressed the importance of respite services, counselling, and including carers as part of the care team. Mental health and emotional wellbeing were raised frequently, including during dialysis and post-transplant.
Funding, structures, and reform
Many discussions pointed to the need for sustainable funding to support programs, workforce initiatives, and wraparound care models. Participants suggested flexible funding structures, philanthropic partnerships, and reforming current funding mechanisms. Several attendees also raised the importance of redefining how system performance is measured, including KPIs and dashboards that reflect equity in access and outcomes. National coordination and planning were described as essential to avoid duplication and improve impact.
Prevention, early intervention, and long-term care
Participants strongly advocated for a whole-of-life approach to kidney care, from early prevention to long-term support post-transplant. Community-led screening programs, diabetes management, and school-based education were suggested strategies. Attendees also stressed the importance of chronic disease management tools, wraparound care, and improved transitions between paediatric and adult kidney services. Housing insecurity and post-transplant continuity of care were noted as significant barriers to maintaining health.
Actions
The following actions come from suggestions provided throughout the three days of the Gathering

Identified Actions to be Taken, Grouped by Theme
Resources and Patient Education
- Develop a minimum set of information that every patient being worked up or on the waitlist should receive, in language that is clear and understandable
- Create transplant education resources adaptable by each transplant unit, with patient videos as core components
- Work with NIKTT to develop and share culturally grounded and engaging pre- and post-transplant care resources
- Use traffic light systems to explain kidney function and test results in a patient-friendly way
- Produce A–Z dialysis induction booklets that cover the full journey, including aftercare and warnings
- Translate resources into local languages and ensure accessibility for both patients and families
- Implement early education about transplant—before dialysis starts—and include culturally appropriate content for children and young people
Workforce Development
- Establish a national network or community of practice for Aboriginal health workers in kidney care
- Fund and embed roles for Aboriginal transplant educators, peer navigators, and cultural liaison officers in dialysis and transplant services
- Elevate the Indigenous health worker role to a senior leadership position, ensuring it is valued and visible
- Recruit more Aboriginal and Torres Strait Islander health workers across services, including in paediatric kidney care
- Partner with workforce agencies to train, mentor, and support regional staff working across the kidney care pathway
Cultural Safety
- Make cultural safety training mandatory in all services (e.g. annual in-person “Walking in Two Worlds” courses)
- Implement and standardise the Clinical Yarning model nationally across nephrology and transplant services
- Include First Nations clinicians in planning and delivery of clinical education and service models
- Address institutional racism and ensure safe, culturally welcoming environments for patients and staff
Access and Navigation
- Establish mobile dialysis trucks and increase dialysis chairs in rural and remote communities
- Fund and deliver home dialysis training and support to enable return to Country
- Provide transport assistance and accommodation support for patients travelling for treatment
- Support earlier transplant workup at CKD stage 4, including screening in schools and communities using outreach vans
- Ensure post-transplant support is available in regional areas
Systems and Strategy
- Create a national transplant scorecard to monitor and report outcomes by site and population group
- Use NIKTT to coordinate national pooling of resources, sharing adaptable tools and templates across jurisdictions
- Develop and implement a national action plan for transplant equity with defined drivers and accountability
- Collaborate with TSANZ, OTA, ANZSN, and governments to align funding, strategy, and implementation efforts
- Host regular national Gatherings to build capability, monitor progress, and share learning
Advocacy and Governance
- Establish a national body to represent Aboriginal and Torres Strait Islander people with kidney disease and transplantation
- Raise awareness of this work in an ongoing and visible way to keep transplantation equity on the agenda
- Strengthen and expand patient reference groups and Indigenous Reference Groups to inform service delivery
- Ensure funding transparency, so communities know how decisions are made and what is achieved
Position Statement
The Position Statement was reviewed and edited to ensure it remains fit-for-purpose

Updated during the 2025 NIKTT Gathering on Kaurna Yarta, Adelaide, 18-20 February 2025.
Delegates attending the 2025 NIKTT Gathering support the continued strategic efforts by Aboriginal and Torres Strait Islander peoples, in partnership with advocates, to advance Aboriginal and Torres Strait Islander peoples’ rights to optimal health and wellbeing through equitable and accessible kidney transplantation.
The delegation, as listed online, endorses the following recommendations to improve care before and after kidney transplantation:
- Establishment of a body that leads national efforts to improve care, develops resources, advocates for change, shares knowledge, and monitors research and service delivery;
- Ongoing support and career development opportunities for the Aboriginal and Torres Strait Islander kidney health workforce, including nurses, doctors, allied health professionals, patient navigators, transplantation coordinators, Aboriginal liaison officers, and Aboriginal health practitioners;
- The implementation and expansion of wrap-around support services, including support groups and patient reference groups;
- Aboriginal and Torres Strait Islander people experience healthcare free of racism, through ongoing cultural awareness, training, safety, and accountability;
- Relevant education and sharing resources created that are designed by and delivered by Aboriginal and Torres Strait Islander people;
- Transparency of information in an understandable and accessible way, supporting family decision making for live kidney donation and transplantation;
- Young peoples’ kidney health and wellbeing prioritised and improved through transplantation, in the next phase of strategic transplantation equity work;
- Identify and address the unmet needs of carers, adult patients, children and young adults, and elders navigating transplant access and care
The delegation endorses the rights of self-determination and leadership by Aboriginal and Torres Strait Islander peoples who are best positioned to understand the needs of their own communities.
The delegates find it crucial that improving kidney failure outcomes through transplantation means partnering effectively with existing health services. Delegates also support the safety and rights of all workers, ensuring the right to work without oppression and racism (overt and convert), as a key foundation of successful partnerships.
Delegates understand that kidney health, including care during kidney replacement therapy, is just one part of overall kidney care and healthcare. It must be supported by a range of services that focus on health and well-being as a whole. To improve health outcomes, individual efforts require their own funding and governance, led by Aboriginal and Torres Strait Islander leadership. We acknowledge that without appropriate resources, others may struggle to partner in this work. The NIKTT has learned, through equity and access projects, that improving transplantation equity requires additional funding that isn’t covered by current service procedures.
The delegation therefore endorses the following actions for the next phase of the work to improve transplantation equity:
- Establishing a body to represent Aboriginal and Torres Strait Islander peoples living with kidney disease and transplantation, which will oversee and support networks, resources, reporting, monitoring, and accountability;
- Ongoing development of programs to facilitate better access to transplantation with a focus on improving the health of people with CKD so they can be waitlisted;
- Monitoring, recording, and reporting on improvements in workforce, program delivery, and transplant waitlisting and achieved transplantation;
- Working with workforce partners to grow an experienced, culturally safe, and resourced Aboriginal and Torres Strait Islander regional workforce across all levels of prevention, transplant access and post-transplant care in Community-controlled health services;
- Promoting transparency and accountability of funding, data, and information about kidney health services so that we can know how decisions are made, by whom, and what has been achieved;
- Continuing to host Gathering meetings that raise awareness and facilitate the capabilities of national networks.
A full list of the delegates who officially endorsed the Statement is available on the NIKTT website.

Next Steps

The 2025 Gathering set out clear priorities for improving kidney transplantation access and outcomes for Aboriginal and Torres Strait Islander people. These include establishing a formal First Nations-led governance body, investing in defined workforce roles such as transplant educators and navigators, and producing consistent, culturally relevant patient education materials. Participants also emphasised the importance of transparent data and reporting mechanisms to track progress, and the need for accountability across services and jurisdictions.
The outcomes of the Gathering will be submitted to the Federal Department of Health, Disability and Ageing to inform implementation of Priority 2 of the National Strategy for Organ Donation, Retrieval and Transplantation. A full report and the endorsed Position Statement are available online.
We encourage readers to:
- Access the reports, Position Statement, and Community priorities and share with colleagues and networks
- Get in touch with the NIKTT Secretariat to discuss opportunities for collaboration
- Advocate for the resourcing and implementation of the NIKTT recommendations through the National Strategy and locally
The next phase of work will depend on continued national coordination, government commitment, and meaningful partnerships with Aboriginal and Torres Strait Islander communities. We look forward to continuing to progress this work with you.
We extend our heartfelt thanks to the patients, carers, and all attendees who travelled to Kaurna Yarta to take part in the 2025 Gathering. Your voices, experiences, and leadership were at the centre of this event. We also acknowledge the tireless efforts of the support teams and NIKTT staff who worked behind the scenes to make the Gathering possible.
We gratefully acknowledge the Australian Government Department of Health, Diability and Ageing for funding the National Indigenous Kidney Transplantation Taskforce.
We thank the Transplantation Society of Australia and New Zealand (TSANZ) for their ongoing partnership and commitment to improving transplantation equity.
We also thank our Gathering sponsors — Astellas and Vantive — for their generous support of the event.


Thank you